Alzheimer's disease (AD) is characterized by the abnormal accumulation in the brain of the proteins tau and amyloid, the latter constituting amyloid plaques. In its typical form, the disease is revealed by memory disorders. However, the amnestic troubles are not always related to AD and some patients may be misdiagnosed as having AD.
To improve diagnostic accuracy, researchers studied patients who consulted for a memory disorder suggestive of AD : the amnestic syndrome of the hippocampal type (ASHT). Thirty-six patients with progressive ASHT and 30 controls underwent i) a complete neuropsychological evaluation by neurologists of the Service de Neurologie de la Mémoire et du Langage of the Hôpital Sainte-Anne, ii) MRI neuroimaging (ICM, Paris) to measure brain atrophy and iii) a PET neuroimaging assessment performed at the SHFJ (Orsay) using [11C]-PiB (tracer of β-amyloid deposits) and [18F]-Flortaucipir (tracer of tau pathology) to quantify the importance of the accumulation of abnormal proteins, as well as their distribution in the brain. Patients were then followed for 2 years, with a second 3-T MRI and tau PET at the last visit.
The results show that, although all ASHT patients had marked atrophy of the internal temporal regions involved in memory, a fraction of them (15/36) were free of the amyloid and tau deposits characteristic of AD. Follow-up revealed distinct clinical evolutions, with a more marked deterioration of cognitive abilities during the 2 years of follow-up in AD patients, as well as a greater progression in these patients of temporal lobe atrophy and tau protein deposits measured by PET imaging. In some non-Alzheimer's amnesic patients, the use of PET tau imaging has identified a possible non-Alzheimer's tauopathy limited to mnestic regions, which, until then, had only been described in studies involving post-mortem brain examination.
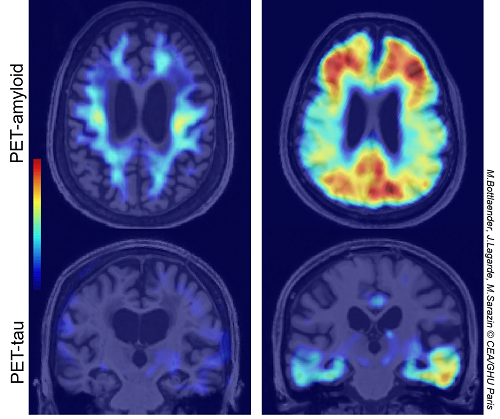 PET-amyloid (top, axial slices) and PET-tau (bottom, coronal slices) images obtained in a non-Alzheimer's amnesic patient (left) and in an Alzheimer's amnesic patient (right) M.Bottlaender, J.Lagarde, M.Sarazin © CEA/GHU Paris
PET-amyloid (top, axial slices) and PET-tau (bottom, coronal slices) images obtained in a non-Alzheimer's amnesic patient (left) and in an Alzheimer's amnesic patient (right) M.Bottlaender, J.Lagarde, M.Sarazin © CEA/GHU Paris
This study reveals the importance of a good characterization of patients who consult for a memory disorder, including the study of the physiopathological processes, to refine the diagnosis of the underlying disease and better anticipate the potential evolution of the cognitive troubles. Amyloid and tau PET imaging demonstrates here all its contribution in this approach. At the dawn of new curative treatments for AD, this step is now essential.
Contacts : Michel Bottlaender (michel.bottlaender@universite-paris-saclay.fr) ; Julien Lagarde (j.lagarde@ghu-paris.fr) ; Marie Sarazin (m.sarazin@ghu-paris.fr)
Note : In accordance with the recent biological definition of AD, its PET signature was defined as the combination of i) a positive cortical amyloid load, and ii) increased retention of the tau tracer in the entorhinal cortex and at least one of the following regions: amygdala, parahippocampal gyrus, fusiform gyrus. Patients who did not fulfill these criteria were considered to have non-AD pathology.